The growing trend of Vaccine Nationalism
Today the World
Health Organization has warned against “vaccine nationalism”, cautioning
richer countries that if they keep treatments to themselves they cannot expect
to remain safe if poor nations remain exposed.
As global cases of
Covid-19 passed
19 million on Friday, WHO chief Tedros Adhanom Ghebreyesus said it would be
in the interest of wealthier nations to help every country protect itself
against the disease.
“Vaccine nationalism
is not good, it will not help us,” Tedros told the Aspen Security Forum in the
United States, via video-link from the WHO’s headquarters in Geneva.
“For the world to
recover faster, it has to recover together, because it’s a globalized world:
the economies are intertwined. Part of the world or a few countries cannot be a
safe haven and recover.
“The damage from
Covid-19 could be less when those countries who... have the funding commit to
this.”
Several countries are
racing to find a vaccine for coronavirus, which has killed more than 700,000
people globally.
There was some good
news as of late, this according to the recent Novavax results. However it is no secret
that Scientists fear that the current pandemic could lead to a geopolitical
fight over vaccines. And that ‘vaccine nationalism’ threatens global plan
to distribute COVID-19 shots fairly.
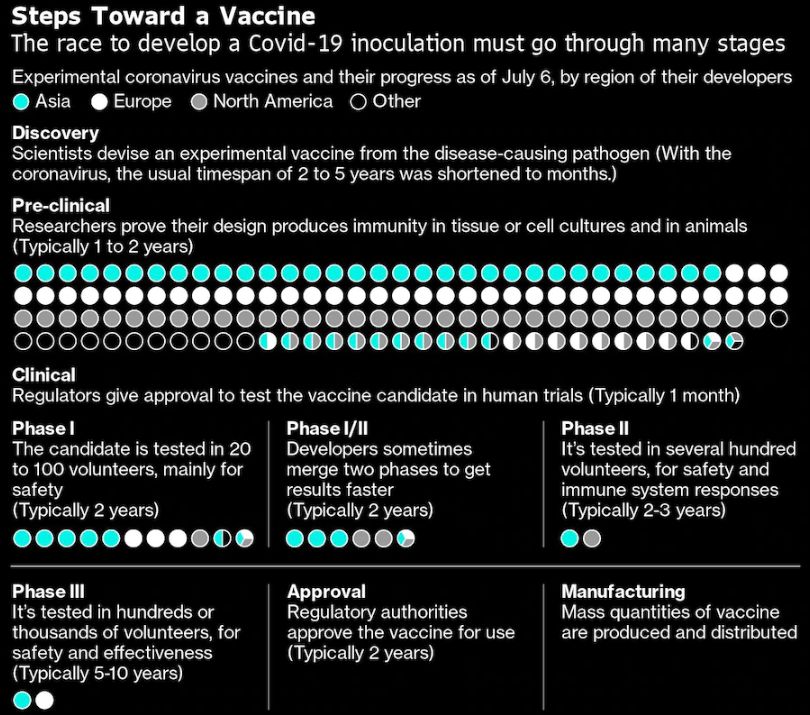
The race
to develop an inoculation against Covid-19, involving vaccine developers in
more
than 30 countries, entails cross-border collaboration but also high-stakes
competition. Some countries are using their research dollars to try to buy the
first place in line for supplies in the event an experimental vaccine proves
effective. Public health specialists warn that such vaccine nationalism could
result in the pandemic lasting
longer, by preventing the most efficient allocation of shots to prevent
Covid-19.
The drug companies
find themselves caught in the middle. While eager to bring products to market
as quickly as possible, they face risks in moving too quickly in order to fit
certain agenda's like for example the US
election calendar
As part of its Operation
Warp Speed aimed at advancing the development of coronavirus
countermeasures, the U.S. has committed billions of dollars of support to
vaccine companies, with the priority being protecting American citizens first.
Officials have placed advance orders for hundreds of millions of doses of
vaccines, in the event they prove effective, with the aim to deliver sufficient
supply to cover the U.S. population by January 2021. The approach is in keeping
with the U.S. government’s purchase of 500,000 doses of the Covid-19 treatment
remdesivir, which is all of the manufacturer’s production for July and 90% for
August and September.

It escaped no one
that the proposed deadline of Operation Warp Speed also intersected nicely with
President Trump’s need to curb the virus before the election in November.
The ensuing race for
a vaccine, in the middle of a campaign in which the president’s handling of the
pandemic is the key issue after he has spent his time in office undermining
science and the
expertise of the federal bureaucracy, is now testing the system set up to
ensure safe and effective drugs to a degree never before seen.
Under constant
pressure from a White House anxious for good news and a public desperate for a
silver bullet to end the crisis, the government’s researchers are fearful of
political intervention in the coming months and are struggling to ensure that
the government maintains the right balance between speed and rigorous
regulation, according to interviews with administration officials, federal
scientists and outside experts.
Who besides the U.S.?
The U.K. has already
secured the
highest number of potential Covid-19 vaccine doses per capita, ahead of the
U.S., having signed a deal with GlaxoSmithKline Plc and Sanofi for as many as
60 million doses. The Serum Institute in India is developing one of the leading
Covid-19 vaccine candidates, and its owner has signaled that most of the
initial supply of a successful shot would be distributed within India. Japan
is trying to lock up supplies, having made a deal with Pfizer Inc. and BioNTech
SE for 120 million doses of the vaccine they’re developing. Germany, France,
Italy and the Netherlands have signed an initial contract for pre-orders of 300
million vaccine doses with AstraZeneca that would be available to all members
of the European Union.
Can vaccine nationalists guarantee first access to a
vaccine?
That depends. What
may prove more important than who has invested in a vaccine is where it is
manufactured. Pharmaceutical companies are preparing for the possibility that
the governments in control of manufacturing locations will demand sufficient
doses to cover their population before allowing exports. This would hardly be
unprecedented. This year, under the pressure of the pandemic, more than 90
states and territories have placed export curbs on medicines and medical
supplies. Anticipating export bans, vaccine developers are working to build
parallel manufacturing facilities in multiple countries, but it’s an expensive
endeavor with large financial risks, given that the vast majority of
experimental vaccines don’t pan out. In its agreements to fund vaccine
developers, the U.S. government has mostly negotiated manufacturing within the
U.S.
Who’s pursuing a different approach?
Three groups -- the
World Health Organization; the Coalition for Epidemic Preparedness Innovations,
which works to advance new vaccines, and Gavi, a global non-profit group
focused on vaccine delivery -- have set up a program aimed at distributing
successful vaccines equitably around the world. Called the Covid-19 Vaccines
Global Access Facility (Covax), it calls on higher
income countries to invest $18 billion in about 12 experimental vaccines and
ensure that early access is shared around the globe when doses become
available. The intended appeal to rich countries is that the facility spreads
their bets across a variety of potential vaccines, any of which individually is
likely to fail. China’s President Xi Jinping has pledged to make any effective
vaccine against the coronavirus that is developed by China, a frontrunner in
the effort, accessible and affordable globally as a “public good.”
What are the prospects for those approaches?
More than 70
countries have indicated an interest in joining Covax,
though none have formally done so. The plan calls for donor countries to commit
by the end of August and provide an advance of 15% of the $18 billion. The
U.S., India and Russia have declined to participate. One issue around China’s
pledge to share any vaccine it develops is quality assurance. A 2018 scandal
that uncovered instances of Chinese vaccine-makers cutting corners in
production has given its industry a bad global reputation. After the incident,
Beijing passed new laws carrying hefty fines to police the industry.
What’s at stake?
Countries taking an
“every nation for itself“ approach are likely to reduce vaccine access for
other countries and drive up prices, leaving poorer nations especially in the
lurch. The concern is that the world will see a repeat of the situation in the
last pandemic, when rich nations purchased all the available supply of vaccines
against the H1N1 flu virus in 2009-10. Who gets access to vaccines and how much
they are willing to pay will have consequences for international relations in
coming years, with vaccines potentially becoming leverage in political
disputes. Beyond that, global health experts say, the pandemic will be
controlled fastest if a future vaccine is deployed in the most efficient way
possible -- with the first doses going to groups around the world that are at
the highest risk, such as medical workers, nursing home staffers and the
elderly, rather than to whole populations in the richest countries.
For updates click homepage here